%20program/full%20time%20study/third%20year/Foundations%20of%20Nursing%20Practicum/19.%20Sleep,%20Comfort.files/image024.jpg)
Poker Chip Pain Assessment Tool Online
| Measure | Brief Description | Ages (years) | Psychometrics | EBA Rating |
|---|---|---|---|---|
| Pain intensity self-report | ||||
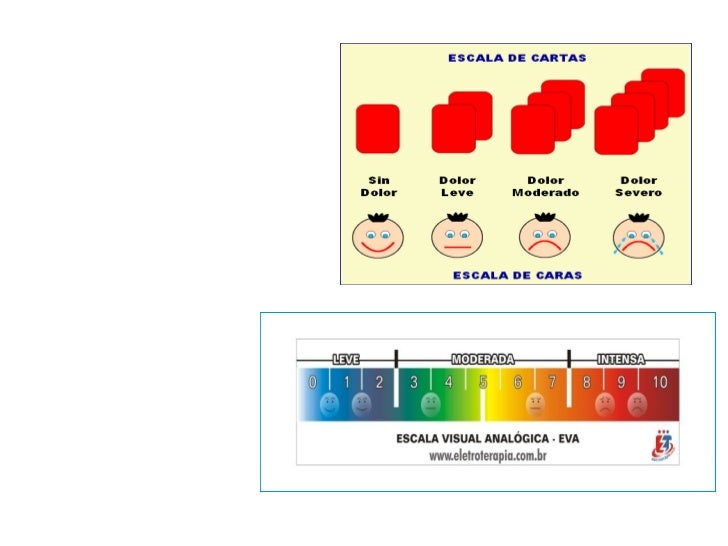
| Visual analog scale (VAS) | Self-report visual analog scales for pain intensity. Horizontal line with descriptive pain anchors at endpoints; draws line that intersects to indicate intensity. | 3–adult | Inter-rater correlations =.28–.72a Concurrent validity =.61–.90 Test-retest reliability =.41–.58 | Well-established |
| The Oucher (Beyer, 1984) | Self-report photograph scale for pain intensity. | 3–12 | Concurrent validity =.62–.95 Test-retest reliability = 78% of children reported scores within ± one level after 15 min. | Well-established |
| Wong-Baker Faces Pain Rating Scale (Wong & Baker, 1988) | Self-report faces scale for acute pain. six line drawn faces range from no hurt to hurts worst. | 3–18 | Concurrent validity: Other pain measures =.67–73 Inter-rater correlations =.26–.37 | Approaching well-established |
| Faces Pain Scale-Revised (FPS-R; Hicks, von Baeyer, Spafford, van Korlaar & Goodenough, 1993) | Self-report faces scale for acute pain. six cartoon faces range from neutral to high pain expression. | 4–16 | Concurrent validity =.84–.99 Inter-rater correlations =.84–.99 | Well-established |
| Poker chip tool (Hester, 1979) | Self-report poker chips are used to represent pain intensity. Child chooses which chips represent the pain they experience | 4–7 | Inter-rater correlations =.23–.70 Concurrent validity =.65–.94 Test-retest reliability (8 hr) =.83 | Well-established |
| Questionnaire and Diaries | ||||
| Headache Diary (Richardson, McGrath, Cunningham, & Humphreys, 1983) | Likert scale used to assess intensity of headache pain four times a day. Scale can be behavioral or subjective | 8–17 | Concordance (weighted κ) =.18–1.0 | Approaching well-established |
| Pain Diary (Hunfeld et al., 2001; Hunfeld et al., 2002) | Visual analogue scale assessing intensity of current pain three times a day | 12–18 (parent proxy 5–11) | Test-retest reliability =.88–.98 Concurrent validity =.46–.84 Convergent validity =.03–.56 | Approaching well-established |
| Abu-Saad Pediatric Pain Assessment Tool (PPAT; Abu-Saad, Kroonen, & Halfens, 1990) | Self-report multidimensional questionnaire of pain using 32 sensory, affective, and evaluative word descriptors, and a 10 cm scale that measures present and worst pain. | 5–17 | Internal consistency =.83 Cross-informant correlations =.28–.92 for child, parent, nurse, physician present and worse pain Concurrent validity =.94–.97 (10 cm);.45–.51 (NWD) other pain measures; Ns 10 cm and Headache Diary Convergent validity =.50–4.50 Discriminant validity =.14–.26 | Approaching well-established |
| Varni-Thompson Pediatric Pain Questionnaire (PPQ; Varni & Thompson, 1985) | Questionnaire that assesses chronic pain intensity, location, sensory, evaluative, and affective qualities of pain via self-report and parent / physician proxy-report. Used with a variety of populations (e.g., JRA, SCD, fibromyalgia). | 5–18 | Test-Retest reliability =.29–.41 Inter-rater correlations =.40–.85 VAS predictive of disability estimates (p <.05) Convergent Validity =.27–.68 with disease status;.06–.45 with psychological functioning | Well-established |
| Behavioral Observation | ||||
| Procedure Behavioral Rating Scale (PBRS; Katz, Kellerman, & Siegel, 1980) | Observational measure of behavioral distress (pain, anxiety, and fear) during painful medical procedures. Thirteen operationally defined behaviors. | 0–18 | Inter-rater reliability =.81–.94 Convergent validity =.33–.68 | Approaching well-established |
| Observational Scale of Behavioral Distress (OSBD; Jay, Ozolins, Elliott, & Caldwell, 1983; OSBD-R, Elliott, Jay, & Woody, 1987) | Observational measure of pain during acute medical procedures. Originally consisted of 11 behaviors that indicate distress, but has been revised to include eight. | 2–20 | Internal consistency =.68–.72 Concurrent validity =.20–.76 Inter-rater reliability = 80–91% | Well-established |
| Child–Adult Medical Procedure Interaction Scale (CAMPIS; Blount et al., 1989; CAMPIS-R; Blount et al., 1997) | Observational measure used to assess child pain during acute medical procedures. Child coping and parent / medical staff behaviors are also assessed. | 2–13 | Inter-rater reliability =.65–.92 for the different scales;.90 for distress (κ) | Well-established |
| Procedure Behavior Checklist (PBCL; LeBaron, & Zeltzer, 1984) | Observational measure of pain and anxiety during invasive medical procedures. Eight operationally defined behaviors rated on occurrence and intensity (scale 1–5) | 3–18 | Inter-rater reliability = 72–94% Convergent validity =.42–.74 | Well-established |
| Children's Hospital of Eastern Ontario Pain Scale (CHEOPS; McGrath, Johnson, Goodman, Dunn, & Chapman, 1985) | Observational measure of postoperative pain in children. | 1–12 | Inter-rater reliability = 95% Concurrent validity =.35–.85 | Well-established |
| COMFORT Scale (Ambuel, Hamlett, Marx, & Blumer, 1992) | Observer rated measure for use in intensive care environments. Includes eight behaviorally anchored rating scales. | 0–18 | Inter-rater reliability =.51–.93 (κ) Concurrent validity =.26–.90 Internal consistency =.90–.92 | Well-established |
| Child Facial Coding System (CFCS; Chambers, Cassidy, McGrath, Gilbert, Craig, 1996). | Observational measure of facial expressions during painful medical procedures. Thirteen facial actions coded for frequency or intensity | 2–5 | Inter-rater reliability =.75–.83 Concurrent validity =.28–.73 | Approaching well-established |
| Premature Infant Pain Profile (PIPP; Stevens, Johnston, Petryshen, & Taddio, 1996) | Observational measure of acute pain in premature infants. Seven indicators of pain | Preterm infants | Internal consistency =.59–.76 Inter-rater reliability =.95–.97 | Well-established |
Child Pain Scale
At Pinecrest, clinicians have used or adapted for use various pain assessment tools, including the Wong-Baker Faces Pain Rating Scale,29 the Poker Chip Tool,26 the Eland Color Scale,9 and the Faces, Legs, Activity, Cry, and Consolability (FLACC) scale.19,27 In some cases, patients have also been asked to draw pictures that reflect their pain.